AC Joint Separation Specialist
The AC joint is the articulation between the medial end of the acromion and the distal (lateral) end of the clavicle. The AC joint is located above the glenohumeral joint (true shoulder joint). Unlike shoulder joint, the AC joint is small and has limited mobility and function. However, it is the main connection between the upper arm and the rest of the axial skeleton. The entire upper extremity “hangs” from the AC joint which is why the coracoclavicular ligaments are also called the suspensory ligament. The primary stabilizer of the AC joint is the short and strong coracoclavicular ligament which has two components (coracoid and trapezoid).
The ligaments that support the AC joint itself, the acromioclavicular ligaments are secondary stabilizers.
A complete separation requires complete failure of both sets of ligaments.
Acromioclavicular Joint (AC Joint) Separation
The more severe the injury the more the joint is disrupted.
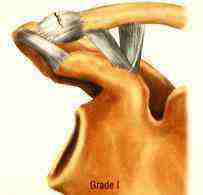
MILD 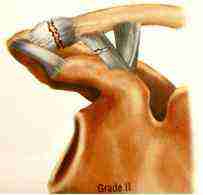
Moderate 
Severe
Symptoms
Complete separation (Grades 3, 4, 5, and 6)
Initial symptoms

An acute shoulder separation usually results from a direct fall on the point of the shoulder. This severe direct force on the supporting ligaments of the AC joint causes these ligaments to fail resulting in a separation of the Acromioclavicular Joint (AC Joint). In severe cases, both the acromioclavicular ligaments as well as the coracoclavicular ligaments are ruptured, and there is an immediate deformity that occurs. Without surgery this deformity remains permanent as the entire weight of the arm continues to pull the acromial side of the injury downward. Depending on the severity of the injury this deformity can be quite dramatic as the joint can be pulled apart as much as two inches. Initially the primary symptoms of this injury are pain, weakness, and deformity.
For more in-depth information on AC Joint Separation Grading.
Complete separation (Grades 3, 4, 5, and 6) – Late symptoms
After the symptoms of the initial trauma subside, some patients may go on to have pain-free and satisfactory function of the shoulder, although the deformity will always be present.
In a majority of patients, however, the mismatch of the joint will create on going and disabling symptoms. These include localized pain, painful clicking and popping, and shoulder fatigue. Active patients such as those involved in manual labor, repetitive tasks or athletes may notice either a generalized weakness or lack of endurance. While physical therapy may overcome some of these symptoms, the permanent derangement of the anatomy leaves the shoulder function compromised for many patients.
Stable or incomplete separation (Grades 1 and 2) – INITIAL SYMPTOMS
In less severe case the anatomy is left either somewhat (Grade 2) or completely intact (Grade 1). Any amount of deformity even in incomplete ruptures will be permanent for the reasons mentioned above. Pain can be quite severe even in cases with little deformity; however, simple treatment with a sling for comfort, ice, rest, and early rehab will result in resolution in most cases.
Late symptoms
In some cases of incomplete separation or even in cases with normal x-rays there can be persistent symptoms. The initial impact may cause cell death of the articulating cartilage of the joint causing late breakdown of cartilage tissue. This type of traumatically induced arthritis can cause chronic pain and require surgical treatment in rare cases. Fortunately, a repair or reconstruction is rarely indicated and a simple debridement of the end of the clavicle will reproducibly resolve these symptoms.
Treatment Timing
Timing of surgery is critical as the procedure for an acute repair is much simpler than the reconstruction required for a chronic separation.
Acute repair

Once an AC joint has a complete separation, the deforming forces of the arm (downward) prevent any chance of reducing the dislocation, much less the proper healing of the torn ligaments. The primary goal of an acute repair is to reduce the deformity with a mechanical device so that the tissues can heal. An acute disruption of the ligaments provokes an intense healing response in the body. If the bones can be brought into alignment and held there reliably, natural ligament healing can occur. In the early period after a complete separation, the ends of the ligaments can also be sewn together reinforcing and adding to the body’s healing response. Early attempts to do this with simple screw fixation were largely successful; however, the rigidity of this construct did lead to hardware breakage and occasion slippage. Our technique is extremely strong and rigid in the direction of the deformity but allows for motion in other planes. Thus ligament healing can occur without overly constraining the anatomy.
The technique is simple, restores the anatomy to its original state, and requires no grafting or other tissue transfer. Once the initial period (about 3-6 weeks) of healing response has passed, however, a more complex procedure is required.
Chronic repair
Once the initial period of healing response has passed the torn ligaments ends scar up into contracted lumps of scar tissue and the injury site no longer has the biologic ability to heal. In this setting, new ligament tissue has to be brought into the repair site and sewn into place, requiring an extended period of healing and tissue incorporation before it can function normally. In these cases the coracoclavicular ligament (CA ligament) is detached from the acromion and swiveled over to the front of the clavicle where it is surgically reattached. This supplies ample vascularized tissue that can initiate a healing response around the ligament resulting in a very thick growth of scar tissue that forms between the clavicle and the coracoid stabilizing the AC joint. Alternative techniques involve the use of a donor tendon graft (cadaveric tissue) but this is rarely necessary except in circumstances of revision surgery. While removing the end of the clavicle is often recommended with other techniques, this is rarely necessary as it carries the risk of weakening the repair site and adds more complexity to the procedure.
Surgical Decision Making
Deciding whether or not to have early surgery is a complex decision in many cases. For cases of very severe deformity (type 4 and type 5 separations) and for extremely active patients surgery is strongly recommended. In those less active or with only a type 3 separation, decision making needs to be individualized. It is difficult to predict ahead of time which patients will be satisfied without surgery and which won’t. An unsuccessful attempt at nonsurgical treatment does, however, result in the need for a more complex surgical procedure. Therefore, each patient will have to consider their needs and expectations carefully before deciding on what is best for them.
Technique
GROUND BREAKING AC Joint Separation surgery technique by Dr. Steven Struhl

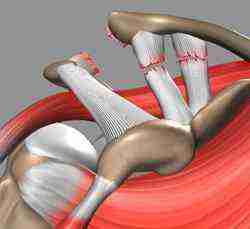
The joint is reduced to its anatomical location and held in place with two small plates (endobuttons) connected by a continuous loop of extremely strong suture. The course of the device is anatomically placed and there are no knots, eliminating the possibility of knot slippage.
Technique detail

Because of the powerful deforming forces disrupting the AC joint, the repair technique must be extremely strong in the direction of the deforming forces yet flexible in other planes to allow for normal shoulder movement. This is accomplished by connecting two small metal plates (endo buttons) with a continuous loop of suture. This unique construct eliminates any “weak links” in the system providing reliable stability during the time it takes for the body to provide true biological healing.
Exposure
A small incision (1-2 inches) is made over the front of the shoulder, exposing the top of the clavicle and the top of the coracoid. It is not necessary to cut any muscle off the bone. The deltoid muscle is simply split in line with its fibers in order to visualize the repair size. With a downward force the distal clavicle is reduced so that it lines up with the acromion.
Bone preparation
A drill hole is made in the clavicle and then into the coracoid process. This drill hole is in the same location as the native (but torn) coracoclavicular ligament.
Endo button passage
The endo button and its associated sutures are then pushed through both drill holes and out the bottom of the coracoid process. Then the endo button is “deployed” so that it seats flush against the underside of the bone. The loop of correct length is then pulled up through the clavicular hole and a second endo button slid under the small bit of loop protruding out the top of the clavicle.
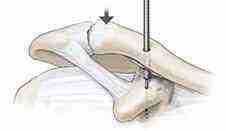
Bone preparation 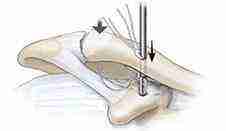
Endo button passage 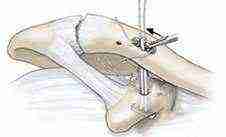
Endo button passage 
Fixation 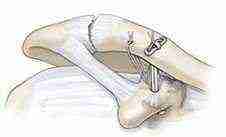
Final Repair
Fixation
Two suture tails that are anchored in the first (coracoid) endo button are now passed through opposite holes of the second (clavicular) endo button. The endo button is now seated flat on top of the clavicle and the sutures tied on top, thereby holding this endo button into place. A second suture is passed into a separate drill hole in between the main drill hole and the AC joint and tied giving additional fixation and stability.
Final Repair
At this point the torn acromioclavicular and coracoclavicular ligaments are sutured and tied, providing additional fixation and recreating the original anatomy.
Dr. Struhl’s article
Read Dr. Struhl’s published article on Double Endo button Technique for Repair of Complete Acromioclavicular Joint Dislocations
Contact our practice today to schedule your consultation with Dr. Struhl.
Please Visit Dr. Struhl’s AC Joint Separation Website for more information regarding AC Joint Separation Treatment